Pudendal Neuralgia in a Nutshell
- Goneuptothesky

- Jan 31, 2021
- 4 min read

Although this condition is relatively easy to obtain from working out, many people haven't even heard of it. This is rather unfortunate and simply not ok. If there is anything we can do in our daily lives to avoid chronic pain we absolutely should be informed about it to make wise choices to steer clear of those consequences. That is why I wanted to give a synopsis on Pudendal Neuralgia: in case you currently fear it, are seeking a diagnosis for it, or are trying to treat it.
What is it? Pudendal Neuralgia, also known as pudendal nerve entrapment or Alcock's canal syndrome, is a pelvic pain condition which can occur in the vulva, perineum, or deep in the pelvis. The type of pain depends on the person but can feel like burning, shooting, itching, aching, or raw anywhere in the clitoris, labia, urethra, vagina, anus, rectum, or between them. It can even extend down the legs and into the feet since the same level of the spinal cord supplies that skin where your brain perceives the pain. This pain stems from the pudendal nerve that runs between your pubic and tail bones, which is why not everyone feels it in the same place or as many places. This can lead to dyspareunia, but also pain from simply sitting too long, bending, stooping, or laying the wrong way while sleeping.
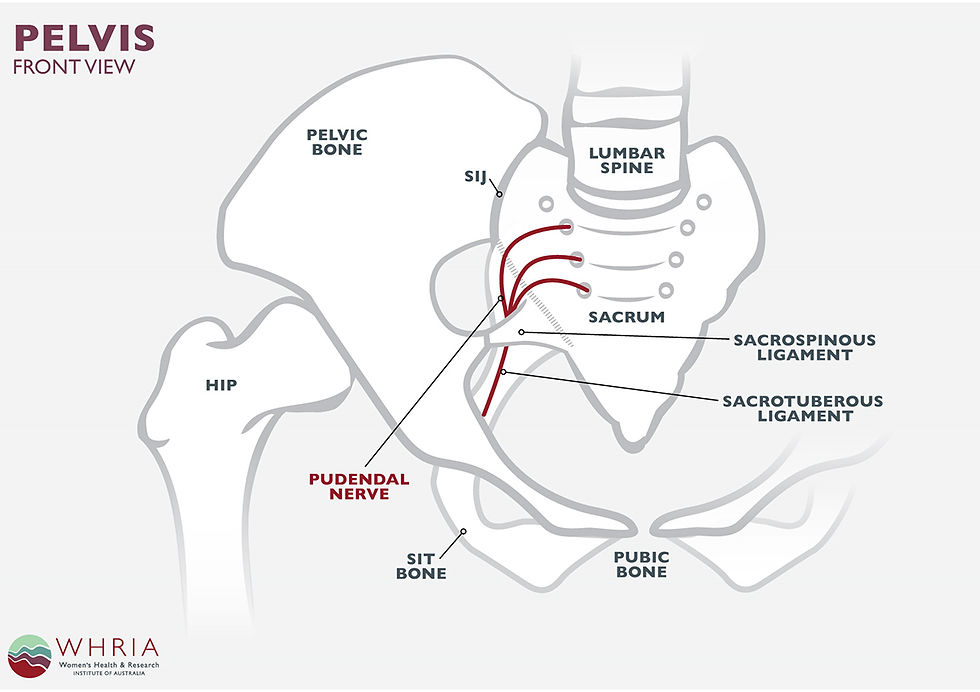
How do you get it? Pudendal Neuralgia, much like sciatica, usually comes about from damage or trauma to the nerve, but stress, poor posture, and straining exacerbate the issue, so you want to be careful and aware of what you're doing in the gym and the bathroom. The pudendal nerve travels a narrow pathway between ligaments, ridges of the pelvis, and the pelvic floor muscles, starting at the sacrum below the spine's base. From there it disperses into three branches, to the clitoris, labia, and rectum. Along this route, two points are susceptible to injury: where the nerve goes between the sacrospinous and sacrotuberous ligaments and where it goes between the pelvic floor and ischial spine (referred to as the Alcock's canal). This can be caused by making the following mistakes. Stretching a nerve past 15% of its normal length can cause permanent nerve damage, which could occur from childbirth or doing deep squats while holding weights. Compression injury happens from blocking the blood flow to the area, which could occur from bicycle riding on a saddle-nose seat. Excessive inflammation from infections such as Lyme disease or herpes can lead to an inflamed pudendal nerve. Surgeries like hysterectomies, laparoscopic surgery, or vaginal prolapse surgery can end up causing pudendal nerve injury since they are involving the reproductive organs in that area. Traumas like a major fall onto the butt or sacroiliac joint of course can also upset the pudendal nerve. And finally, entrapment caused by tight pelvic floor muscles or thickened ligaments can lead to pudendal nerve pain.
How do you diagnose it? In order to solidify Pudendal Neuralgia as the cause of your pain, your doctor will want to run a few tests and review your medical history to determine what caused it and thus how to fix it. A digital vaginal exam can reveal this condition by a positive Tinel's sign, which means tapping the nerve internally created a pins and needles type of sensation on the perineum. A quantitative sensory test will use vibrations and temperature variations to recognize any changes to the nerve structure or fiber damage. During a pudendal nerve motor latency test a trained technician at a neurology office will insert a gloved finger into the vagina or rectum with an electrode on the tip. This sends a weak electrical current through the nerve and the speed is recorded through a a small needle inserted into the perineum to test for entrapment or damage. Electromyography can be somewhat painful, but this test identifies any loss of nerve conduction by evaluating the electrical activity from the urethral and sphincter muscles after inserting a two-needle or fine wire electrode into the muscle and recording the level of activity. A given test, your doctor will probably want to do a pudendal nerve block to see if that reduces the pain or not. Next, they may do a Pudendal MRI to see the structures surrounding the nerve. If needed, they may also want to do a sonography (ultrasound) of the sacroiliac joint and ligaments or one of the pelvic floor muscles. Once everything has been fully assessed your doctor can decide if this is truly the condition you are suffering from and where to go from here.

How do you treat it? As with all pelvic issues, Pudendal Neuralgia has no perfect cure for all people, but many options you can try to see what works best for you. Taking pressure off of the pudendal nerve helps provide some pain relief. Thus, lying down, standing, sitting on a donut pillow or toilet seat can give some immediate, temporary comfort. As for more long term fixes, however, you may want to seek out a physical therapist for a good stretching regimen and possibly dilators if you are experiencing pain with sex. Some people experience relief from acupuncture, deep tissue massage, nerve pain meds, anti-depressants, Botox injections, a TENS machine or herbs. Others resort to surgery to cut the sacrospinous or sacrotuberous ligaments to relieve the pressure. You may also require a counselor to help manage the emotional pain brought on by carrying the physical pain day by day. Lifestyle changes go a long way in coping with these kinds of conditions, but they only work if you keep at them, which can be extremely difficult if you are dealing with depression and wanting to give up. That's why it's so important to approach the problem from all angles and seek out whatever help you need so professionals can not only hold you accountable but also be an ear to listen when you need to rant or have someone in the know empathize with your situation. For helpful info from other women suffering with this condition on Instagram, follow the accounts @thepelvicwarrior and @pelvichealthguru. For more general info on this condition you can go here. Remember, you are not alone in tackling this issue and there are many others out there if you are looking for support!



Comments